Accessing medical care in Gaza has always been a challenge, made worse by the onset of the current conflict. But now we are in dire straits.
Of the 36 hospitals once functioning, 19 are left — all with limited capacity. Our two field hospitals are among the five still standing on the Gaza strip. This is a drop in the ocean to serve the 2.1 million population that remain, who have been displaced many times over.
Yet, UK-Med hospitals are still treating 1000 people each day. On Monday, three babies were born in the maternity unit of our Al-Mawasi field hospital, two by emergency c-section.
Their births represent a slither of hope among the chaos.
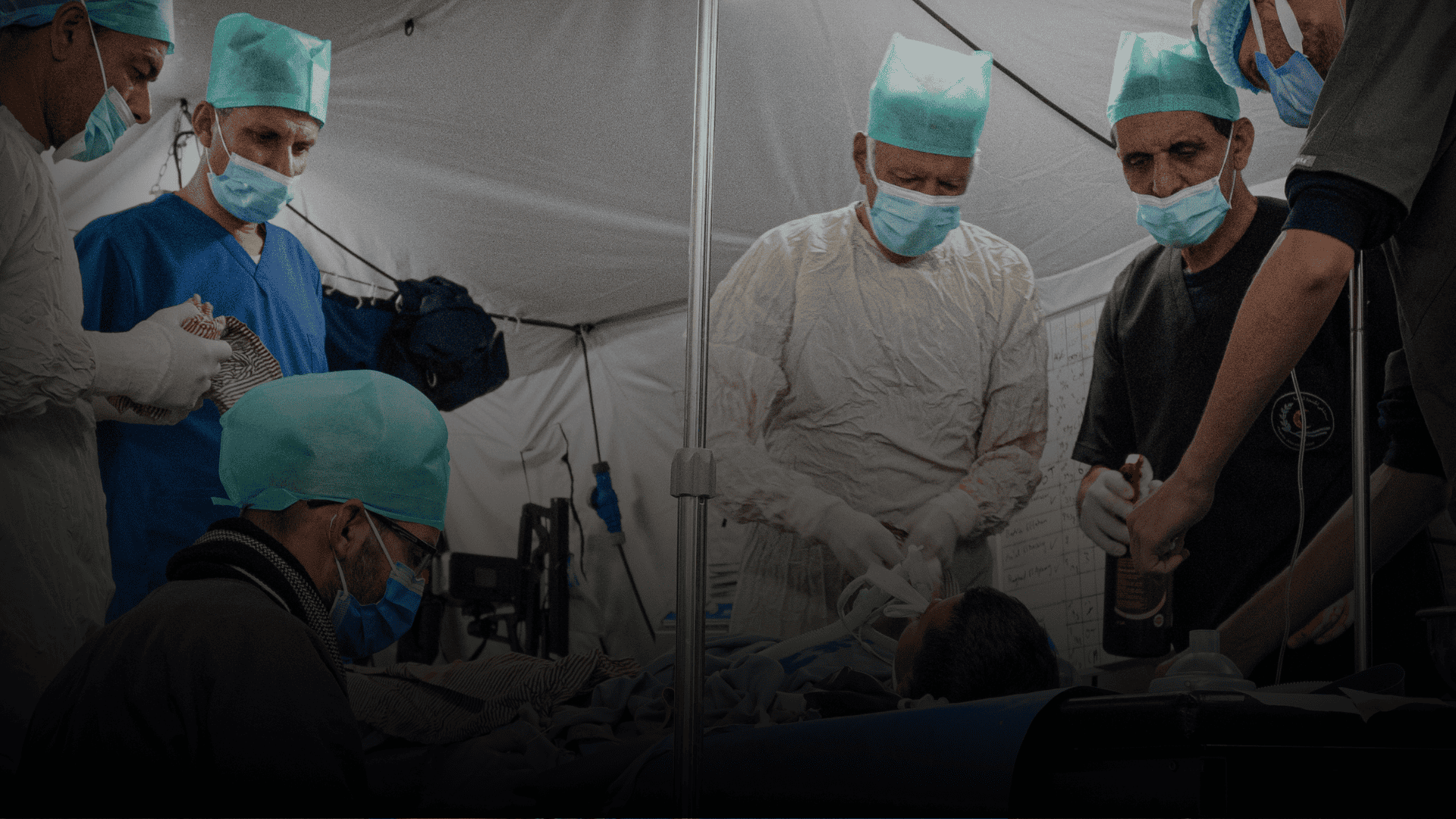
More and more people are arriving at our hospital doors; supplies are running out, our team are rationing painkillers and antibiotics, and our operating theatres are overrun by repeated mass casualty incidents, bringing many wounded people into the facilities.
“This is the largest and most sustained humanitarian medical operation UK-Med has ever undertaken,” said David Wightwick, CEO of UK-Med.
“We’re not talking about our field hospitals closing — but without further funding, our ability to continue supporting frontline care at this scale is at risk. We urgently need public support to sustain this work.”
Our team has taken the time to speak with the media about the situation on the ground – two excerpts follow and links at the bottom of the page:
“I was in Gaza last year and didn’t think it could possibly get any worse… but it has”: Mel Graham, UK-Med nurse from Elderslie, Renfrewshire.
“That first night the ceasefire shattered was easily the worst thing I have ever experienced. Even though we knew it was coming, it was still such a shock.
“The sound of explosions and fighting were so close to the hospital, so we knew we were going to be busy. At maybe two or three in the morning the first casualties started coming in. It was a conveyor belt of carnage.
“My role involved triaging patients. Amongst that first load of patients brought in, there was a two-year-old girl dead on arrival.
“There wasn’t a mark on her and I just remember standing there thinking ‘How can this happen?’. She looked completely perfect and was just covered in a thick layer of dust.
“It’s different when you are dealing with people with visible injuries. With some blast injuries there are no obvious signs externally, but the shockwave had fatally affected her tiny wee lungs.
“The porters went to get a body bag for her, but the shortage of aid getting in meant there were only adult body bags available. She just disappeared into it.
“We took her to the temporary mortuary at the back of the hospital. We put two chairs out for the family to come in… but no-one ever came. I fear her parents had obviously been killed too.”

Mel added: “The sight of that little girl will haunt me forever. It is the thing that I think about most. It’s at the forefront of my brain. It is not natural for a child to die like that.
“I didn’t want to leave her there alone, but I had to get back to help the many other casualties who had been rushed in.”
Foreign Secretary David Lammy has been leading calls for more aid to enter Gaza and urgently wants to see a return to the ceasefire. Over 50,000 people have now been killed and more than 90% of the population displaced from their homes.
“This was the worst”: Dr. Iain Lennon on providing medical care in Gaza
Dr. Iain Lennon, an Emergency Medicine Consultant with 25 years of experience working in the NHS, finds himself once again at the centre of a humanitarian catastrophe. Working with UK-Med, Dr. Lennon has previously responded to the Rohingya crisis in Bangladesh and the COVID-19 pandemic. But nothing quite prepared him for this.
“So about midnight on Saturday,” he recounted, “a piece of ordnance fell in one of the tented camps about half a kilometre away from us. As a result, both ourselves and a number of the other hospital organisations in the region had a mass casualty incident where we received very high numbers of severely injured patients.”

Dr. Lennon and his team saw 27 patients that night. “There was another 16 or so dead on arrival at the hospital. We were seeing significant wounds – amputations, injuries to the abdomen, shrapnel wounds – a wide range of really quite serious injuries.” It was, his colleagues told him, “the worst event that they’ve had since the field hospital here has opened.”
While some of the most critically injured were transferred to Nasser Hospital Complex, where UK-Med is also running the Emergency Department, Dr. Lennon’s team has been operating around the clock. “Our theatre staff have been working non-stop since this morning… to remove shrapnel and to manage some of the broken bones.”
Despite reports of burns, he noted, “we didn’t actually see a significant number of burns at all. We think, unfortunately, those people never made it out of the camp.”
As Gaza’s northern hospitals collapse – “we believe that they’re all very much non-functional”- Dr. Lennon’s team is taking in stabilised patients from Nasser Hospital. “Our ward is fairly much at capacity at the moment.”
Meanwhile, local staff face staggering obstacles. “They’re still struggling. Our staff are coming from as far north as Gaza City itself and traveling on donkey carts and motorcycles… which is something like a three-hour transit for them. They find that an additional stress on top of the fact that they are then separated from their families and they don’t entirely know what’s going on with them.”
UK-Med in Gaza:
Since January 2024, UK-Med has been operating emergency two field hospitals across Gaza, treating nearly half a million patients in response to the ongoing humanitarian crisis. Their facilities are staffed by a dedicated mix of international and local healthcare professionals working under extremely dangerous and resource-scarce conditions. Funded through a combination of institutional donors such as FCDO and WHO and public donations, UK-Med’s operations are a critical lifeline in a region where formal healthcare infrastructure has been badly impacted.






